BIMONTHLY ASSIGNMENT - MAY 2021
Note: I have been assigned the following cases to solve the related questions in an attempt to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, diagnosis and the treatment regimen.
Note: The information in this assignment has also been obtained from various sources that I have referenced and acknowledged with their online links and I have paraphrased them further. However the images I have borrowed may have copyright issues as they may not be certified through a creative commons license in which case, I hope the original authors will get in touch with me and I shall remove them if they wish.
CARDIOLOGY
Case 1
ANSWERS TO CASE 1

In heart failure with preserved ejection fraction (HFpEF), the left side of your heart is too stiff to fully relax between heartbeats. That means it can't fill up with enough blood to pump out to your body. High blood pressure and other conditions that make your heart work harder are the main causes of heart failure with preserved ejection fraction. Conditions that stiffen the chambers of the heart such as obesity and diabetes are also causes of this type of heart failure. Over time, your heart muscle thickens to adapt, which makes it stiffer.
Diagnosis: An echocardiography measures the patient's ejection fraction. Your ejection fraction is the percent of the blood in the lower left chamber of your heart (the left ventricle) that is pumped out of your heart with each heartbeat. Ejection fraction indicates how well your heart pumps. This helps to diagnose the type of heart failure and guide treatment.
- If 40% or less of the blood in the left ventricle is pumped out in one beat, it is heart failure with reduced ejection fraction.
- If 50% or more of the blood in the left ventricle is pumped out in one beat, it is heart failure with preserved ejection fraction.
- If ejection fraction is somewhere in between (41% to 49%), maybe diagnosed with heart failure with borderline ejection fraction.
REFERENCES:
- https://www.nhlbi.nih.gov/health-topics/heart-failure
In case of pericardial effusion in this patient which was 20.7 mm at admission and resolved to 14mm by discharge date.
Pericardiocentesis for diagnostic purposes is not justified in cases of mild or moderate effusions (<20 mm) for the following reasons
Without hemodynamic compromise, pericardiocentesis is indicated for:
None of the above criteria were met by our patient as confirmed by investigations.
2004 ESC guidelines1 support the use of pericardiocentesis if purulent, tuberculous, or neoplastic pericarditis is suspected. Pericardiocentesis can also be performed for patients with persistent symptomatic pericardial effusions.
Pericardiocentesis is also the management for cardiac tamponade which was not detected in this patient.
Post-infarction rupture of the free wall is a contraindication to needle pericardiocentesis due to the potential risk of aggravating the myocardial rupture via rapid pericardial decompression and restoration of systemic arterial pressure - due to potential past MI ?
- https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-15/Pericardiocentesis-in-cardiac-tamponade-indications-and-practical-aspects
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2878263/
- Age - Patient is 78 years. People 65 years or older have a higher risk of heart failure because aging can weaken and stiffen your heart.
- Lifestyle habits - Patient is a chronic smoker + alcoholic, which increases his risk of heart failure.
- Comorbidities - Patient is a K/C/O Diabetes Mellitus and Hypertension.
- Previous MI? Pericardial and pleural effusion? - leading to pericarditis?
- https://www.nhlbi.nih.gov/health-topics/heart-failure
Case 2
ANSWERS TO CASE 2
- Obesity - Central Truncal
- Diabetes Mellitus
- Chronic Kidney Disease - Stage 4 in this patient.
- Hypertension
- Atrial Fibrillation
- Anemia - HB was 7.5gm/dl with normochromic normocytic anemia
- Chronic smoking and alcohol intake.
- Age - 73 years.

- Fluid backs up into these areas because the heart is not filling adequately. The buildup of fluid in the lungs can result in shortness of breath while fluid in the legs caused swelling/pedal edema in this patient.
- https://www.umcvc.org/conditions-treatments/heart-failure-preserved-ejection-fraction-hfpef
- https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.119.313572
- Causes of anemia in CKD may include:
- Inflammation
- Low levels of EPO (erythropoietin) due to kidney damage as kidney is the main source of EPO.
- Low levels of the nutrients needed to make red blood cells.
- Shortened red blood cell survival.
- The elevation of proinflammatory cytokines plays an essential role in insulin resistance and induces the appearance of cardiovascular complications diabetic micro- and macrovascular, kidney disease and anemia.
- By increasing especially IL-6, anti-erythropoietic effect occurs, since this cytokine changes the sensitivity of progenitors to erythropoietin (erythroid growth factor) and also promotes apoptosis of immature erythrocytes causing a decrease, further, in the number of circulating erythrocytes and consequently causing a reduction of circulating hemoglobin
- https://www.niddk.nih.gov/health-information/blood-diseases/anemia-inflammation-chronic-disease
- https://jasn.asnjournals.org/content/23/10/1631
- https://www.hindawi.com/journals/anemia/2015/354737/
- Leading to the hypothesis of an underlying associated local sub-basement membrane-zone connective-tissue alteration and micro-angiopathy causing blisters/blebs.
- These are a spontaneous, distinct, non-inflammatory, blistering condition of the skin predominantly seen in patients with diabetes mellitus.
- Lesions have a predilection for the distal lower extremities more than the upper extremities, especially the tips of the toes and plantar surfaces of the feet - as in this patent on the 3rd toe of left foot.
- Wound healing occurs as a cellular response to injury and involves activation of keratinocytes, fibroblasts, endothelial cells, macrophages, and platelets. Many growth factors and cytokines released by these cell types are needed to coordinate and maintain healing.
- Risk factors are primarily related to hypoglycemic conditions associated with antidiabetic therapy, which include:
- Decreased or impaired growth factor production.
- Angiogenic response.
- Macrophage function.
- Collagen accumulation.
- Epidermal barrier function.
- Quantity of granulation tissue.
- Keratinocyte and fibroblast migration and proliferation.
- Number of epidermal nerves.
- Bone healing.
- Balance between the accumulation of ECM components and their remodeling by MMP
| Local Factors | Systemic Factors |
|---|---|
|
|
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1857239/
- https://bjdabcd.com/index.php/bjd/article/view/52/120#:~:text=Diabetic%20bullae%2C%20also%20known%20as,reported%20in%201930%20by%20Kramer.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2903966/
- https://www.diabetes.co.uk/news/2018/dec/four-stages-of-type-2-diabetes-identified-by-us-doctors99311412.html#:~:text=The%20statement's%20four%20stages%20of,%2C%20or%2C%20related%20microvascular%20events.
Case 3
ANSWERS TO CASE 3
- https://www.nhs.uk/conditions/atrialfibrillation/causes/#:~:text=The%20exact%20cause%20of%20atrial,atherosclerosis
- β1-agonist
- Indicated for the Congestive cardiac failure that the patient presented with.
- Sustained improvement of cardiac function in patients with congestive heart failure after short-term infusion of dobutamine.
- Reference: https://pubmed.ncbi.nlm.nih.gov/6357536/
- Digitalis glycosides
- Indicated for the Congestive cardiac failure that the patient presented with.
- The goal of digoxin therapy in patients with congestive heart failure is to improve quality of life by reducing symptoms and preventing hospitalizations.
- Reference: https://www.aafp.org/afp/2000/0715/p409.html
- Anticoagulant
- Reduces the risk of thrombi formation and embolization in atrial fibrillation.
- Reference : https://www.ahajournals.org/doi/full/10.1161/hq0701.093686
- Vasodilatory Non-selective Beta Blocker
- Indicated for Atrial fibrillation, hypertension, heart failure.
- Escalating doses of oral carvedilol can be effectively and safely used in the acute treatment of AF with fast ventricular rate.
- Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4231552/
- Mucolytic, for NSAID abuse??
- Also it is a free radical scavenger which could reduce the oxidative stress in atrial fibrillation?
- Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3331849/#:~:text=An%20increasing%20body%20of%20evidence,of%20postoperative%20AF%20(POAF).
- The therapeutic effect of oral anticoagulants (OACs) is measured by monitoring the prothrombin time.
- OAC dosage must be adjusted to achieve a narrow range of the desired prothrombin time values, usually expressed as the international normalized ratio (INR).Thromboplastins, the essential reagent for prothrombin time testing.
- Oral Anticoagulant
- Indicated in Atrial Fibrillation
- prevention of the intrahepatic metabolism of vitamin K epoxides, and an induction of vitamin K deficiency. As a result, thrombin generation slows, and clot formation becomes impaired due to decreased biologic activity of the prothrombin complex proteins.
- Significant stroke reduction in primary and secondary prevention and Significant reduction in total mortality compared to placebo.
- Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1768341/
- Risk factors include: hypertension, diabetes, elderly age, and prior history of heart or renal failure. NSAID Abuse could have caused Renal dysfunction in this patient.
- The pathophysiology of the cardiorenal syndrome involves intrarenal hemodynamics, trans-renal perfusion pressure and systemic neurohormonal factors, compromise of the net renal perfusion pressure, inadequate cardiac output and decreased perfusion pressure.
- In the presence of risk factors such as hypertension as this patient, there is further reduction of glomerular filtration.
- Neurohumoral activation mediated by activation of arterial baroreceptors and intrarenal sensors. These reflexes lead to the activation of the renin-angiotensin system, sympathoadrenal system and arginine-vasopressin system – an intrinsic self-defense system to maintain blood pressure and intravascular volume.
- All of these factors will lead to peripheral and intrarenal vasoconstriction, further decreasing renal blood flow and GFR, and leading to a decrease in renal function.
- The consequences also lead to renal hypoxia, inflammation, cytokine release, and progressive structural and functional loss.
- The net clinical consequences are sodium and fluid retention, increased urea, uric acid and creatinine levels and progressive reduction of renal function.
The patient has Cardiorenal syndrome type 4
Due to the involvement of Cardiovascular System with primary renal disease, with Ventricular hypertrophy and diastolic dysfunction.

Pathophysiological pathways of type-4 cardiorenal syndrome. It has been highlighted the role of uremia in developing minor and major cardiovascular complications referring to main CKD-related cardiovascular risk factors such as secondary hyperparathyroidism, anemia, accelerated atherosclerosis and chronic inflammation.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2794438/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5415026/
- Hypertension
- Old age
- Male gender
- NSAID abuse? leading to renal disease
International normalized ratio (INR)
- It is the preferred test of choice for patients taking vitamin K antagonists (VKA).
- It can also be used to assess the risk of bleeding or the coagulation status of the patients.
- Patients taking oral anticoagulants are required to monitor INR to adjust the VKA doses.
- The INR is derived from prothrombin time (PT) which is calculated as a ratio of the patient’s PT to a control PT standardized for the potency of the thromboplastin reagent developed by the World Health Organization (WHO) using the following formula:
- INR = Patient PT ÷ Control PT
- It is the most commonly used test for laboratory monitoring of unfractionated heparin therapy
- Laboratory monitoring is widely recommended to measure the anticoagulant effect of unfractionated heparin and to adjust the dose to maintain levels in the target therapeutic range.
- The focus of clinicians who manage unfractionated heparin therapy should be to ensure that an adequate starting dose of unfractionated heparin is used and that the aPTT method is standardized.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1768341/
- https://www.ncbi.nlm.nih.gov/books/NBK507707/
- https://pubmed.ncbi.nlm.nih.gov/8725715/
- https://pubmed.ncbi.nlm.nih.gov/17080209/#:~:text=Laboratory%20monitoring%20is%20widely%20recommended,partial%20thromboplastin%20time%20(aPTT)
Case 4
ANSWERS TO CASE 4
- MOA- Loop diuretics such as Torsemide induce its effect by competing with chloride to bind to the Na-K-2Cl (NKCC2) cotransporter at the apical membrane of the thick ascending limb of the loop of Henle and blocking the cotransporter, which inhibits the reabsorption of sodium and chloride. By inhibiting NaCl reabsorption, tonicity in the interstitium decreases, and free water excretion increases as a result.
- Advantages of Torsemide over other loop diuretics:
- Torsemide is known to have the longest half-life at 3 to 4 hours and can be as long as 5 to 6 hours in patients with renal/hepatic dysfunction or heart failure.
- Torsemide provides the longest duration of action and can give even greater diuretic effects in patients that have hepatic dysfunction or heart failure.
- https://www.ncbi.nlm.nih.gov/books/NBK546656/
Case 5
- https://www.ncbi.nlm.nih.gov/books/NBK470572/
- Tab. ASPIRIN 325 mg PO/STAT
- Salicylate, NSAID
- Indicated to reduce the blood clot formation in coronary artery in Inferior wall MI in this patient.
- Aspirin used for secondary prevention of atherothrombotic events.
- Tab ATORVAS 80mg PO/STAT
- Statin, HMG Co-A reductase inhibitor, decreased cholesterol production.
- Indicated to reduce FFA's, has anti-inflammatory and antithrombotic effects too in MI.
- Free fatty acid levels showed a sharp increase during the acute phase of MI. Treatment with atorvastatin 20 mg/day, and especially with 40 mg/day, resulted in a decrease in free fatty acid levels. The positive effect of low-dose atorvastatin (20 mg/day) is normalization of the adipokine status. Administration of atorvastatin 20 mg/day was accompanied with a statistically significant reduction in glucose levels (by 14%) and C-peptide levels (by 38%), and a decrease in the homeostasis model assessment of insulin resistance index on day 12.
- Tab CLOPITAB 300mg PO/STAT
- Antiplatelet drug, blood thinner
- Addition of Clopidogrel to aspirin reduces the risk of major ischemic events by up to a further one-third in patients with STEMI treated with fibrinolytic therapy and undergoing percutaneous coronary intervention, with no significant increase in bleeding. Thus, dual antiplatelet therapy with the combination of clopidogrel and aspirin is becoming the new standard of care for the management of patients with STEMI.
- Inj HAI 6U/IV STAT
- Human Actrapid Insulin used to reduce high blood sugar levels in diabetes patients.
- Fast acting, Insulin infusion improves myocardial blood flow in the ischemic and non-ischemic regions in subjects with type 2 diabetes.
- Angioplasty with stent placement
- Angioplasty is a procedure to open narrowed or blocked coronary arteries that supply blood to the heart.
- A coronary artery stent is a small, metal mesh tube that expands inside a coronary artery. A stent is often placed during or immediately after angioplasty.
- Coronary intervention techniques like angioplasty and stent placement reproduce reperfusion in a significant number of patients.
Reference: https://pmj.bmj.com/content/75/888/591
- The concomitant use of primary angioplasty and thrombolysis (facilitated angioplasty) is considered experimental and has no place in routine management of acute MI at this time.
- Best outcomes occur when primary PCI is performed with a door-to-balloon time of < 90 minutes and when symptoms onset was < 12 hours. Primary PCI is only indicated when symptoms duration is 12-24 hours (delayed presentation) if severe congestive heart failure, hemodynamic/electrical instability or continued angina is present. Primary PCI is not recommended when symptom onset is more than 12 hours and the patient is asymptomatic (OAT trial).
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3387753/
- https://www.healio.com/cardiology/learn-the-heart/cardiology-review/topic-reviews/coronary-artery-disease-stemi/treatment-revascularization
Case 6
- https://www.verywellhealth.com/non-st-segment-elevation-myocardial-infarction-nstemi-1746017#:~:text=In%20NSTEMI%2C%20considered%20the%20%22intermediate,damage%20is%20far%20less%20extensive.
- Tab. MET XL 25 MG/STAT.
- Metoprolol, Selective Beta 1 receptor blocker.
- Beta blockers reduce myocardial workload, and thus oxygen demand, via a reduction in heart rate and blood pressure. They reduce catecholamine levels, decrease myocardial ischemia and limit infarct size, and may prevent the development of definite infarction in acute coronary syndrome (ACS) patients.
- All hemodynamically stable AMI patients receive BB to reduce chest pain, as well as to reduce the risk of re-infarction and Ventricular arrhythmias. There may be a slight reduction in mortality if the patient has not previously been treated with BB.
- Acute ST-elevation myocardial infarction (STEMI)
- Primary PCI is the recommended method of reperfusion when it can be performed in a timely fashion by experienced operators.[1]
- STEMI and ischemic symptoms of less than 12 hours' duration.[2]
- STEMI and ischemic symptoms of less than 12 hours' duration and contraindications to fibrinolytic therapy
- PCI improves survival in patients with significant (>50%) stenosis
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Early invasive therapy (within 2 hours of symptoms) recommended with refractory angina, recurrent angina, symptoms of heart failure, new or worsening mitral regurgitation, hemodynamic instability, or sustained ventricular tachycardia/fibrillation.
- A worsening of troponin levels should trigger an early therapy (within 24 hours)
- Unstable angina
- Stable angina
- Anginal equivalent (e.g., dyspnea, arrhythmia, or dizziness or syncope)
- High-risk stress test findings
- PCI is indicated for the critical coronary artery stenosis, which does not qualify for coronary artery bypass surgery (CABG).
Absolute Contraindications:
- Noncompliance with the procedure and inability to take dual antiplatelet therapy.
- High bleeding risk (thrombocytopenia, peptic ulcer, severe coagulopathy)
- Multiple percutaneous coronary intervention restenosis.
Relative Contraindications:
- Intolerance for oral antiplatelets long-term
- Absence of cardiac surgery backup
- Hypercoagulable state
- High-grade chronic kidney disease
- Chronic total occlusion of SVG
- An artery with a diameter of <1.5 mm
- Stenosis of <50%
- Critical left main stenosis with no collateral flow or patent bypass graft.
- https://www.ncbi.nlm.nih.gov/books/NBK556123/
- The reinfarctions were not only procedural-related infarcts (i.e., early procedural enzymatic leaks), but true ST elevation reinfarctions that accumulated throughout follow-up. One explanation for the trend toward an increase in reinfarctions with PCI may be embolization resulting in myocardial damage and impaired collateral flow.
- Dangerous side effects due to over-prescription and over-medicalization.
- Release of pharmaceuticals into the environment as, for example, in case of over- and misuse of antibiotics, thus contributing to the proliferation of antimicrobial resistance.
- Psychological effects - unnecessary fear, resulting in increased sense of vulnerability and psychological suffering.
- Drug Dependence
- Economic burden - Cost involved in over diagnosis and overtreatment of many diseases will make it difficult to keep healthcare systems financially viable. There is also direct relation between overtreatment and under-treatment, as there is risk of limited resources being redirected and shifted away from those who need them most.
- https://emcrit.org/pulmcrit/avoiding-over-diagnosis-and-over-treatment-of-mi-in-critically-ill-patients/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7586591/
- https://www.acc.org/latest-in-cardiology/clinical-trials/2011/10/30/23/23/oat
NEPHROLOGY
Case 1
ANSWERS TO CASE 1
- Hyperactive
- Impulsive Behaviour
- Inattentiveness at school
- Excessive fast talking leading to incomprehension of speech
- Embarrassment associated with the Overactive Bladder.
- Isolating oneself with gadgets as in this patient, the 8 year old was addicted to smart phone and low self esteem.
- Lack of social life stemming from lack of interaction with peers and adults, leading to loss of social activities.
- The child might not notice how his behavior affects other people. He may interrupt a lot and even bug people by breaking social rules.
- With ADHD sometimes he may lose track of a conversation or get distracted by unrelated thoughts and may also misinterpret what others are saying.
- The boy can also have trouble with planning and follow-through. That can lead other people to think he can’t be counted on when doing group projects in schools or other activities.
- https://www.understood.org/en/learning-thinking-differences/child-learning-disabilities/add-adhd/5-ways-adhd-can-affect-social-skill
- Diabetes - Lab Investigations normal, no urine sugars or ketone bodies or any other abnormalities. CUE normal.
- Medications - Except for occasional constipation medication, no other history of any drug intake.
- Urinary Tract Infection - No history of UTI, Urine culture and sensitivity negative for microorganisms and showed no growth.
- Obstructive Sleep Apnea - History of sound and undisturbed sleep
- Anatomical Abnormality - USG Abdomen normal
- https://www.healthline.com/health/overactive-bladder/overactive-bladder-night#takeaway
- https://www.mayoclinic.org/diseases-conditions/bed-wetting/symptoms-causes/syc-20366685
- The goal of evaluation should be to distinguish neurological and anatomical causes from functional causes of bladder dysfunction.
- A thorough history of voiding symptoms and a Bladder diary are essential components to assessment, directing targeted investigation and treatment.
- As all investigations in this child have come out normal, the differential is directing at ADHD, psychosomatic causes or stress related and hence the most common modality for treatment is Behaviour modification and therapy.
- Behavioural Therapy including:-
- Reassurance and Relaxation is very important to calm the child and prevent any stressor from triggering this manifestation.
- Parenting skills training and Education teaches parents the skills they need to encourage and reward positive behaviors in their children and about various approaches.
- Stress management techniques and Counselling can benefit parents of children with ADHD and the patient by increasing their ability to deal with frustration so that they can respond calmly.
- Support groups can help parents and families connect with others who have similar problems and concerns.
- Oxybutynin: Oral. First-line option.
- Ditropan 5 mg Tablets - For 5–12 years, oral, initially 2.5 mg twice daily; if needed, gradually increase to 5 mg 2 or 3 times daily.
- Transdermal route, Oxytrol patch- off label <12 year old can be used if patient can’t swallow or can’t tolerate oral oxybutynin. Do not cut or divide patches as drug release characteristics may be affected.
- https://www.rch.org.au/clinicalguide/guideline_index/Urinary_Incontinence_-_Daytime_wetting/
- https://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder-adhd-the-basics/
- https://www.stlouischildrens.org/conditions-treatments/pollakiuria
Case 2
ANSWERS TO CASE 2
- Hydroureteronephrosis 🠆 retention of urine 🠆 infection with E.coli + presence of pus cells(as detected in investigations) 🠆 urosepsis.
- During TURP, the wide plexus of venous sinuses is often opened and the excess absorption of the irrigation fluids which are highly hypotonic into the bloodstream causes a group of symptoms and findings that is called TURP syndrome.
- Absorption of the irrigation fluid (2000 ml or more) used to expand the operating field and to wash away debris and blood, causing hypoosmolality and dilutional hyponatremia may lead to TURP syndrome which could have been the cause for neurological symptoms such as drowsiness and excessive sleep in this patient.
- The symptoms are generally caused by an excessive fluid load in circulation.
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/transurethral-resection-of-the-prostate-turp
- https://www.mayoclinic.org/tests-procedures/turp/about/pac-2038488
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4543890/
- https://pubmed.ncbi.nlm.nih.gov/29424875/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4220352/
- Diabetes leading to sediment in urine due to kidney injury.
- Urosepsis/ UTI leading to foamy urine.
- Retrograde ejaculation secondary to TURP as a complication and diabetes as an added factor.
- Dehydration ?
- Proteinuria? due to diabetes and kidney injury
- https://www.healthline.com/health/foamy-urine
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6372866/
- https://www.nhs.uk/conditions/transurethral-resection-of-the-prostate-turp/risks/
- Prostate size > 45g ( pt's was 60 gm).
- Immunocompromised state due to Diabetes Type 2 diagnosed 5 years back.
- Size of opened venous sinuses?
- Higher absorption of irrigation fluid and usage of excess amounts?
- Longer resection time?
- Bleeding during procedure?
- Excess hypotonic IV fluids administration?
- Hyponatremia-TURP syndrome - Due to absorption of excess of irrigation fluid during surgery, leading to fatigue and excessive drowsiness the next day.
- Acute Tubular Necrosis - Acute Kidney Injury (high risk) due to using distilled water as an irrigant for TURP causing hemolysis, especially in patients with larger prostates as this patient whose prostate was 60g and with longer resection times.
- Non Oliguric Renal Failure - Due to increasing azotemia (creatinine levels) in this patient (5.2 mg/dl) despite a normal or increased urine output.
- Post-op Infection - Causing pus cells in urine, raised creatinine.
- https://www.karger.com/Article/FullText/342965#:~:text=Bacterial%2C%20viral%20or%20fungal%20infections,be%20due%20to%20multiple%20factors.
- https://pubmed.ncbi.nlm.nih.gov/29424875/
- https://pubmed.ncbi.nlm.nih.gov/16863013/
- https://www.goldjournal.net/article/0090-4295(76)90334-4/pdf
- https://www.nhs.uk/conditions/transurethral-resection-of-the-prostate-turp/risks/
GASTROENTEROLOGY
Case 1
ANSWERS TO CASE 1
- https://shc.amegroups.com/article/view/5553/html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4896175/
- It is the paradoxical clinical deterioration attributable to recovery of immune system while receiving highly active antiretroviral therapy (HAART) for the treatment of human immunodeficiency virus (HIV) infection.
- Deterioration is due to restoration of the patient's capacity to mount an inflammatory immune response against both infectious and noninfectious antigens.
- Human immunodeficiency virus (HIV) infection is associated with immune activation and depletion of CD4T cells, which leads to defects in immune responses. The use of combination antiretroviral therapy (ART) is associated with repletion of circulating CD4T cells and improvement in immune function, which results in a decrease in the incidence of opportunistic infections. However, some individuals experience clinical disease associated with a prominent inflammatory response to an opportunistic pathogen, such as TB bacteria in this patient after commencing ART.
- A retrospective radiologic review of cases revealed worsening radiographs in 45% of patients with infections like TB having increased lymphadenopathy, lobar consolidations, and pleural effusions.
- The chances of IRIS increase with - Clinical worsening including prolonged fever of >101.5 °F, increasing respiratory symptoms, increasing lymphadenopathy.
- Infection with tuberculosis 🠆 immune suppression 🠆 reversible with anti-MTB therapy.
- Systemic Corticosteroids have been used in anecdotal reports with good success at preventing further damage when HAART-mediated inflammation threatens vital structures, especially in Tb infection.
- Another intervention is opted to delay the onset of HAART until anti-MTB therapy has decreased the load of organisms.
- The use of pharmaceutical interventions other than steroids has been limited. Mild cases of inflammation of TB might respond to nonsteroidal anti-inflammatory drugs (NSAIDs), which could be used by themselves or in conjunction with corticosteroids.
- The use of other anti-inflammatory therapies, such as thalidomide, is currently being investigated.
- https://journals.lww.com/mdjournal/Fulltext/2002/05000/Immune_Reconstitution_Inflammatory_Syndrome_.5.aspx
- https://err.ersjournals.com/content/29/158/200094
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2813111/
Case 2
ANSWERS TO CASE 2
- Presenting features of patient - Right hypochondriac pain with symptoms of toxemia including, high grade fever with chills and rigor.
- Laboratory tests indicating impaired liver function - Elevated ALP, Elevated Bilirubin, Hypoalbuminemia, Hypoproteinemia, which have further led to jaundice and pedal edema.
- Could lead to development of spontaneous local peritonitis as a complication, for which characteristic features seen in this patient are - Abdominal Pain, Abdominal distention, Fever, Low urine output, Inability to pass stool or gas, Guarding.
- Presence of a thick collection in right sub-diaphragmatic space could be a sub-diaphragmatic abscess associated with Peritonitis and liver pathology.
- Complete Blood Picture with leukocytosis and neutrophilia also indicate inflammation.
- https://www.mjdrdypu.org/article.aspissn=09752870;year=2017;volume=10;issue=6;spage=532;epage=535;aulast=Bhatia
- https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-020-00858-w#:~:text=6%2C%2018%5D.-,Spontaneous%20gas%2Dforming%20pyogenic%20liver%20abscess%20(GFPLA)%20is%20a,Previous%20studies%20showed%20that%20E.
- https://www.mayoclinic.org/diseases-conditions/peritonitis/symptoms-causes/syc-20376247
- Internal bleeding
- Sepsis 🠊 Shock 🠊 Organ Failure (following septic peritonitis)
- Myocardial Ischemia
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/peritonitis
- https://www.sciencedirect.com/science/article/abs/pii/S0011393X96800981
- https://jemds.com/latest-articles.php?at_id=10191
- Marie Griffin, MD, professor of preventive medicine at Vanderbilt University, says the risk is considerably higher for older adults, especially for women who frequently take the drugs for persistent pain.
- NSAIDs can reduce the amount of blood reaching the kidneys, slowing kidney function. Water and salt retention, high blood pressure, and electrolyte imbalances have been linked to NSAIDs’ effect on the kidneys.
- NSAIDs reduce prostaglandin synthesis, with differences in the extent of inhibition of the enzymes COX-1 and COX-2. Selective COX-2 inhibitors are more likely to cause cardiovascular events, whereas less selective NSAIDs are more likely to cause GI bleeds.
- NSAIDs reduce the antiplatelet effect of aspirin and have a thrombogenic effect on platelet function.
- NSAIDs increase systolic blood pressure by 5 mmHg and increase fluid retention.
- https://www.spine-health.com/treatment/pain-medication/potential-risks-and-complications-nsaids#:~:text=Water%20and%20salt%20retention%2C%20high,NSAIDs%20without%20consulting%20a%20doctor.
- https://www.webmd.com/pain-management/news/20030130/when-relieving-pain-raises-risk
Case 3
ANSWERS TO CASE 3
- Trans-diaphragmatic lymphatic blockage
- There may be a disruption of pancreatic duct, leading to the leakage of pancreatic enzymes and the formation of a pancreatico-pleural fistula, more likely to occur if the duct disruption is posteriorly into the retroperitoneum.
- The pancreatic-pleural fistulae secondary to leak and disruption of the pancreatic duct or pseudocyst caused by an episode of acute pancreatitis. The pancreatic enzymes can track up into the mediastinum and then rupture into the pleural cavity either left side or bilaterally and so create a connection between the pancreatic duct and the pleural cavity.
- Exudation of fluid into the pleural cavity from the subpleural diaphragmatic vessels may also cause pleural effusion.
- https://www.scitechnol.com/peer-review/an-unusual-case-of-dyspnoea-in-a-patient-with-chronic-liver-disease-qeSr.php?article_id=7559
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5633324/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6386740/
- One factor could be because of the sympathetic hyperactivity and circulating catecholamines that elevate glucagon.
- Due to microcirculation disorder and inflammation resulting in pancreas edema, ischemia and necrosis hence affecting secretion and excretion of insulin due to damage to Langerhans Islet cells.
- Due to acute metabolic stress similar to that seen in other clinical situations such as sepsis.
- Thus hyperglycemia could hence be the result of a hyperglucagonemia secondary to stress or the result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
- https://link.springer.com/chapter/10.1007/978-3-642-60580-2_11
- https://clinicaltrials.gov/ct2/show/NCT01470885
- Lipase - 118 IU/L
- Amylase - 252 IU/L
- Elevated levels of gamma glutamyl transferase (GGT), aspartate aminotransferase (AST), and alanine aminotransferase (ALT).
- If the AST level is more than that of ALT, a AST/ALT ratio of > 1 some studies have found in more than 80 percent of alcoholic liver disease patients.
- Neutrophilia
- Increased Bilirubin levels
- https://www.journal-of-hepatology.eu/article/S0168-8278(18)32576-5/fulltext#secst095
- https://pubs.niaaa.nih.gov/publications/aa64/aa64.htm
- https://www.sciencedirect.com/science/article/abs/pii/S1521691803000507
- https://www.clinicaladvisor.com/home/features/what-you-should-know-about-acute-pancreatitis/
Case 4
ANSWERS TO CASE 4
- Based on the CECT, the site of abnormality is the abdomen - pancreas behind the peritoneum of posterior abdominal wall , where the pseudocyst is located due to chronic pancreatitis of the pancreas.
- Pleural effusion between tissues lining the chest-wall and lungs
- Pneumothorax in the space between lungs and chest wall.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2653285/
- Oxygen Supply - For mild Hypoxia
- Inj. MEROPENEM TID for 7 days - Broad Spectrum Antibiotic
- Meropenem is as effective as imipenem in preventing septic complications of patients with severe acute pancreatitis.
- Inj. METROGYL 500 mg IV TID for 5 days - Antibiotic
- Systemic Metronidazole is indicated for the treatment of many anaerobic infections which can clinically present
- Inj. AMIKACIN 500 mg IV BD for 5days - Antibiotic
- The use of prophylactic antibiotics in severe alcoholic acute pancreatitis significantly reduces the incidence of severe infection.
- Total Parenteral Nutrition - Feeding Bypassing GI Tract
- Prevents malnutrition and is a key to reduce inflammation, complications and death in acute pancreatitis. It is considered in patients who cannot tolerate enteral nutrition.
- All pancreatic fistulae that developed during the course of the disease spontaneously closed in patients receiving TPN without operation in a mean period of 33.3 days, and all pseudocysts subsided in an average of 18.3 days.
- I.V NS / RL at the rate 12l ml per hour - Fluid replacement for dehydration
- Normal saline (NS) or Ringer’s lactate (RL) may improve mortality rates and decrease development of systemic inflammatory response syndrome (SIRS), especially the latter.
- Inj. OCTREOTIDE 100 mg SC/BD - Somatostatin analogue
- Long-acting analogue of Somatostatin, Octreotide is a potent inhibitor of exocrine secretion of the pancreas, which plays an important role in the pathogenesis of acute pancreatitis. They also have direct anti-inflammatory and cyto-protective effects.
- Inj. THIAMINE 100 mg in 100 ml NS IV/TID - Prophylactic B1 supplementation
- To prevent Wernicke encephalopathy secondary to thiamine deficiency.
- Inj. TRAMADOL in 100 ml NS IV/OD - Opioid Analgesic
- Tramadol is the most effective oral opioid analgesic for reducing pain in chronic pancreatitis
- PANTOP 40 mg IV/OD - Proton Pump Inhibitor
- Pantoprazole as a proton pump inhibitor (PPI) has pancreatic anti-secretory effect and a pronounced inhibitory reactivity towards hydroxyl radicals.
- USG guided Malecot drainage - For peri pancreatic fluid
- Decreased mortality, high success rate and less adverse events rate.
- Intercostal drainage - Pneumothorax
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1458598/
- https://pubmed.ncbi.nlm.nih.gov/14576501/#:~:text=Meropenem%20is%20as%20effective%20as,patients%20with%20severe%20acute%20pancreatitis.
- https://www.hindawi.com/journals/hpb/2010/523468/#conclusion
- https://pubmed.ncbi.nlm.nih.gov/1903137/
- https://pubmed.ncbi.nlm.nih.gov/8829189/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7211526/
- ournals.lww.com/ajg/fulltext/2018/10001/ringer_s_lactate_vs_normal_saline_in_acute.2.aspx#:~:text=Normal%20saline%20(NS)%20is%20the,poor%20outcomes%2C%20compared%20to%20NS.
- https://www.medscape.com/viewarticle/487410#:~:text=Somatostatin%20and%20its%20long%2Dacting,anti%2Dinflammatory%20and%20cytoprotective%20effects.
- https://pubmed.ncbi.nlm.nih.gov/22233960/
- https://www.aafp.org/afp/2008/0301/p661.html#:~:text=There%20is%20consensus%20that%20tramadol,associated%20with%20gastrointestinal%20adverse%20effects.
- https://pubmed.ncbi.nlm.nih.gov/23242019/#:~:text=Pantoprazole%20as%20a%20proton%20pump,the%20course%20of%20acute%20pancreatitis.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4735000/
HEPATOLOGY
Case 1
ANSWERS TO CASE 1
- Male gender.
- Manual laborer - Palm tree climber.
- Tobacco Beedi smoking.
- Socio-economic background
- Lifestyles practices predisposing to high parasitic burden.
- Relatively lower percentage of alcohol (<5%)
- Possibility of microbial contamination due to a lack of distillation process.
- Microbial or parasitic contamination, transmission and infection during preparation and storage of toddy.
- The nonalcoholic content of toddy alters the gut environment and upregulating enzymes, switching latent Entamoeba (EH) to virulence.
- High iron content in Toddy promotes growth and in-vivo invasiveness of EH, an etiological agent in liver abscess causation.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6077556/
- https://onlinelibrary.wiley.com/doi/full/10.1002/jgh3.12137
- Possible route of spread - Portal transmission or Hematogenous spread or direct spread from biliary system.
- Possible pathology - Bowel content leakage and peritonitis or any intra abdominal infections.
- Makkar et al. have suggested that high iron content of traditional fermented beverages and iron overload due to chronic alcoholism could also lead t
- A high microbial burden due to poor sanitation and immunosuppressive effects of alcohol could render the host more vulnerable to infections. Thus, both the host factors as well as contents of toddy may be responsible for the pathogenesis of liver abscess.
- https://www.worldwidejournals.com/indian-journal-of-applied-research-(IJAR)/recent_issues_pdf/2016/October/October_2016_1492168550__175.pdf
- https://www.researchgate.net/publication/250212621_Pyogenic_Liver_Abscess_and_Indigenous_Alcohol
- https://www.ijph.in/article.aspissn=0019557X;year=2019;volume=63;issue=1;spage=89;epage=90;aulast=Kumar#:~:text=Amoebic%20liver%20abscess%20(ALA)%20is,and%20the%20occurrences%20of%20ALA.&text=Toddy%20is%20a%20local%20alcoholic%20beverage%20consisting%20of%20fermented%20palm%20juice.
- https://www.ncbi.nlm.nih.gov/books/NBK538230/#:~:text=50%25%20of%20solitary%20liver%20abscesses,liver%20lobe%20or%20caudate%20lobe.
- Abscess size of 9.7 x 9.4.
- Clinical deterioration - Elevation of ALP, transaminases, Bilirubin and Low Albumin signifying impaired liver function.
- To test the culture and antibiotic sensitivity and identify the causative organism.
- Failure of clinical improvement of symptoms.
- https://surgical.medresearch.in/index.php/ijoso/article/view/88/176
Case 2
ANSWERS TO CASE 2
- Ingestion of contaminated food or water.
- Toddy consumption.
- Male gender having higher occurrence.
- Lifestyle or hygienic practices.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3014521/
- Inj. ZOSTUM 1.5 gm IV BD: Zostum is a combination medicine of 2 Antibiotic drugs - Sulbactam (penicillin) and Cefoperazone (cephalosporin) to treat Bacterial Infection.
- Inj. METROGYL 500mg IV TID: Metrogyl is an anti-infective medicine comprising of an Antibiotic Metronidazole to treat Bacterial/Parasitic Infections (Amoebic).
- The clinical presentation of both Amoebic and Pyogenic Liver Abscess is indistinguishable.
- Patients usually present with fever and right upper quadrant tenderness.
- Laboratory tests abnormalities such as in this patient showing leukocytosis, increased alkaline phosphatase (ALP) and abnormal liver and renal function tests are often present in both and cannot differentiate effectively.
- Even, imaging techniques, such as ultrasonography and computed tomography (CT) scanning, are useful in demonstrating a space occupying lesion and confirm only the presence or absence of a liver abscess but may not reliably differentiate between PLA and ALA.
- https://www.ncbi.nlm.nih.gov/books/NBK430832/
- https://academic.oup.com/bmb/article/132/1/45/5677141
- Fine needle aspiration for culture is the gold standard for diagnosis of PLA(pyogenic).
- Blood cultures, Entamoeba serology, liver abscess aspirate for culture, molecular and antigen testing also help in reaching a definite diagnosis.
- New potential marker such as Pyruvate Phosphate Dikinase in the form of a lateral flow assay shows potential in the diagnosis of ALA (amoebic).
- Presumptive diagnoses of amoebic (n=471; 82%) vs. pyogenic (n=106; 18%) abscess were based upon amoebic serology, microbiological culture results, and response to therapy.
- Patients with amoebic abscess were more likely to be young males with a tender, solitary, right lobe abscess (P=0.012).
- Univariate analysis found patients with pyogenic abscess more likely to be over 50 years old, with a history of diabetes and jaundice, with pulmonary findings, multiple abscesses, amoebic serology titres <1:256IU and lower levels of serum albumin (P<0.04).
- Multivariate logistic regression analysis confirmed that age >50 years, pulmonary findings on examination, multiple abscesses, and amebic serology titres <1:256IU were predictive of pyogenic infection.
- https://academic.oup.com/bmb/article/132/1/45/5677141
- https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-3156.2004.01246.x
PULMONOLOGY
Case 1
ANSWERS TO CASE 1
• Mechanism of Action:
-Binds to 50S ribosomal subunit of susceptible microorganisms and blocks dissociation of peptidyl tRNA from ribosomes, causing RNA-dependent protein synthesis to arrest and does not affect nucleic acid synthesis.
• Therapeutic Indications:
- Acute exacerbation of COPD due to possible infectious etiology.
• Efficacy over Placebo:
- COPD, azithromycin taken daily for 1 year, when added to usual treatment, decreased the frequency of exacerbations and improved quality of life.
• Mechanism of Action:
- Amoxicillin binds to penicillin-binding proteins, thus inhibiting final transpeptidation step of peptidoglycan synthesis in bacterial cell walls and addition of clavulanate inhibits beta-lactamase-producing bacteria, allowing amoxicillin extended spectrum of action.
- For possible infectious etiology of COPD.
• Efficacy over Placebo:
- Patients with exacerbations of mild to moderate COPD have a higher rate of cure when given amoxicillin/clavulanate compared with placebo.
• Therapeutic Indications:
- Patient's oxygen saturation was 75% at room air.
• Mechanism of Action:
- Chest physiotherapy involves a number of physical techniques to help remove excess mucus from respiratory passages and improve breathing. The goal is to help patients breathe more freely and get more oxygen through the blood stream into all parts of the body. Normally, mucus helps lubricate the lungs.
- Dyspnea in patient due to COPD.
Nebulization with:-
1. IPRAVENT respules is indicated as a bronchodilator for the maintenance treatment of bronchospasm and dyspnea associated with acute exacerbation chronic obstructive pulmonary disease (COPD) in this patient.
Ipratropium bromide is an anticholinergic with para-sympatholytic properties. Anticholinergics prevent the increase in intracellular concentration of cyclic guanosine monophosphate (cyclic GMP) caused by the interaction of acetylcholine with the muscarinic receptors on bronchial smooth muscle.
2. BUDECORT respules contains the potent, non-halogenated, corticosteroid, indicated for dyspnea in this patient due to COPD and to inhibit inflammatory cytokine production.
Budesonide is the potent topical anti-inflammatory glucocorticoid that controls these symptoms.
3. What could be the causes for her current acute exacerbation?
Aspen workshop7 defined AECOPD as “a sustained worsening of the patient's condition from the stable state and beyond normal day to day variations, that is acute in onset and necessitates a change in regular medication in a patient with underlying COPD”.
- Respiratory infections including bacteria, atypical organisms and respiratory viruses, 10% are due to environmental pollution.
- Dust exposure in the working environment affects the lung function values and increased the respiratory symptoms among the rice mill workers and patient works in paddy fields.
- Cooking using solid fuels (such as wood, crop wastes, charcoal, coal and dung) and kerosene in open fires and inefficient stoves. And the patient has been using chulha for past 20 years. One in four or 25% of deaths from chronic obstructive pulmonary disease (COPD) in adults in low- and middle-income countries are due to exposure to household air pollution. Women exposed to high levels of indoor smoke are more than twice as likely to suffer from COPD than women who use cleaner fuels and technologies.
- As the patient received LASIX - Furosemide treatment, it could have led to fluid or electrolyte imbalance (hyponatremia, hypochloremic alkalosis, hypokalemia, hypomagnesemia or hypocalcemia) and she showed the respective signs of electrolyte imbalance : weakness, lethargy, drowsiness, muscular fatigue, oliguria.
- Corticosteroids (Includes hydrocortisone) which the patient was administered and could have caused electrolyte imbalance due to mineralocorticoid functions. Corticosteroids can cause hypokalemia and fluid retention.
- As the patient has right heart failure, this may be due to the pathophysiological alterations seen in the heart failure state leading to neurohumoral activation (stimulation of the renin-angiotensin-aldosterone system, sympatho-adrenergic stimulation), and due to the complications of therapy with diuretics, etc. Patients with heart failure may exhibit hyponatremia due to a decrease in water excretion, which may be related to the enhanced release of both angiotensin and vasopressin and can be exaggerated by diuretic therapy. Along with potassium and calcium, magnesium influences cardiovascular function.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2080749/#!po=20.5556
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4019758/
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0231757
https://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health
https://reference.medscape.com/drug/zithromax-zmax-azithromycin-342523#0
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1113909/
https://reference.medscape.com/drug/augmentin-amoxicillin-clavulanate-342474#10
https://reference.medscape.com/drug/lasix-furosemide-342423#0
https://www.google.com/amp/s/www.practo.com/medicine-info/amp/zoryl-1-mg-tablet-12322
https://www.ciplamed.com/content/ipravent-respulesrespirator-solution#pharmacological%20properties
https://www.sciencedirect.com/science/article/abs/pii/S0031940609000868
https://en.m.wikipedia.org/wiki/Glimepiride
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5552828/
https://pubmed.ncbi.nlm.nih.gov/9428832/#:~:text=Results%3A%20Metformin%20improved%20glucose%20variables,to%202000%20mg%20daily%2C%20respectively
NEUROLOGY
Case 1
ANSWERS TO CASE 1
- It could be due to a fracture or trauma leading to a tear in the head or neck blood vessels that lead to the brain, which can be a source of blood clots that cause a stroke.
- Sudden NUMBNESS or WEAKNESS of face, arm, or leg, especially on one side of the body.
- Sudden CONFUSION, trouble speaking or understanding speech.
- Sudden TROUBLE SEEING in one or both eyes.
- Sudden TROUBLE WALKING, dizziness, loss of balance or coordination.
- Sudden SEVERE HEADACHE with no known cause.
Note: Act F.A.S.T. and do the following simple test:
A—Arms: Ask the person to raise both arms. Does one arm drift downward?
S—Speech: Ask the person to repeat a simple phrase. Is the speech slurred or strange?
T—Time: If you see any of these signs, call 9-1-1 right away.
- https://www.stroke.org/en/about-stroke/stroke-symptoms
- https://www.cdc.gov/stroke/signs_symptoms.htm
- https://www.stroke.org/en/about-stroke/stroke-symptoms
- https://www.cdc.gov/stroke/signs_symptoms.htm
The following drugs were used in this patient:
1. Mannitol
- Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
- Mannitol decreases elevated intracranial pressure after stroke and results in increased cerebral perfusion pressure and brain oxygenation in large, hemispheric strokes.
- Reference: ://www.ahajournals.org/doi/pdf/10.1161/01.str.0000078658.52316.e8
- The beneficial effect of statin therapy on the risk of recurrent stroke was due to a reduction in the risk of cerebral infarction, the mechanism of which largely has been attributed to a reduction in LDL cholesterol levels. The lower average LDL cholesterol level achieved in the atorvastatin as compared with the placebo group is consistent with this hypothesis.
- Decreased the risk of stroke, major coronary events, and revascularization procedures. These results support the initiation of atorvastatin treatment soon after a stroke or TIA.
- Statins lower serum cholesterol level by inhibiting hydroxymethylglutaryl-coenzymeA (HMG-CoA) reductase. Statins have been found to improve endothelial function, modulate thrombogenesis, attenuate inflammatory and oxidative stress damage, and facilitate angiogenesis far beyond lowering cholesterol levels . Statins have also been proved to significantly decrease cardiovascular risk and to improve clinical outcome.
- References: - https://www.nejm.org/doi/10.1056/NEJMoa061894#:~:text=In%20conclusion%2C%20in%20patients%20with,after%20a%20stroke%20or%20TIA.- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428028/
- Aspirin, which thins the blood and thereby prevents clots, is currently used to reduce the long-term risks of a second stroke in patients who've had an ischemic stroke.
- Aspirin slows the blood's clotting action by reducing the clumping of platelets. Platelets are cells that clump together and help to form blood clots. Aspirin keeps platelets from clumping together, thus helping to prevent or reduce blood clots.
- During a heart attack, blood clots form in an already-narrowed artery and block the flow of oxygen-rich blood to the heart muscle (or to part of the brain, in the case of stroke).
- References:
- https://www.webmd.com/stroke/news/20000601/aspirin-after-stroke-helps-prevent-another
- https://www.uofmhealth.org/health-library/te7903spec
References: https://jnnp.bmj.com/content/70/suppl_1/i12
- Epidemiological evidence indicates that recent heavy alcohol consumption increases the risk for all major types of stroke, whereas light-to-moderate alcohol intake is associated with a decreased risk of ischemic stroke.
- https://jnnp.bmj.com/content/70/suppl_1/i12https://pubmed.ncbi.nlm.nih.gov/9778594/
- HDL has anti-atherosclerotic and anti-inflammatory properties and is an important component in Atherosclerosis.
- And as this patient had a Low LDL of 33 mg/dl, that could have been contributed as a risk factor.
- Recent evidence suggests that lower HDL-cholesterol (HDL-C) may worsen the atherosclerotic process by promoting inflammation and progression from subclinical lesion to clinical event.

- https://pubmed.ncbi.nlm.nih.gov/21830454/#:~:text=Studies%20have%20demonstrated%20a%20trend,the%20risk%20of%20recurrent%20stroke.
- https://www.ahajournals.org/doi/10.1161/01.str.0000258347.19449.0f
Case 2
Complete details regarding the case are in the mentioned link above.ANSWERS TO CASE 2
1)What is myelopathy hand ?Ans. As this patient has C3 - C6 OPLL which causes narrowing of the spinal canal and compression of the cervical spinal cord. The following sign could be observed:- A characteristic dysfunction of the hand has been observed in various cervical spinal disorders when there is involvement of the spinal cord.
- There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers.
- These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
- The characteristic nature of the sign permits the distinction between myelopathy and changes due to nerve root or peripheral nerve disorder.
- Both uncoordinated finger motion and trick motion of the wrist were more frequent in myelopathy patients than in healthy controls and uncoordinated finger motion was associated with severity of myelopathy
REFERENCES:- https://pubmed.ncbi.nlm.nih.gov/3818752/
- https://pubmed.ncbi.nlm.nih.gov/20354474/
2)What is finger escape ?Ans. The finger-escape sign : lack of adduction and extension of the ulnar fingers.Grading of the finger-escape sign:Grade Fingers Deficiency0 All None1 Little finger Unable to hold adduction2 Little or little and ring Unable to assume adduction3 Little and ring Unable to assume adduction or full extension4 Little, ring and middle Unable to assume adduction orThe following is a link to a video eliciting this sign:https://vimeo.com/517686531REFERENCE:3)What is Hoffman’s reflex?Ans. The Hoffman sign is an involuntary flexion movement of the thumb and or index finger when the examiner flicks the fingernail of the middle finger down.- The reflexive pathway causes the thumb to flex and adduct quickly.
- A positive Hoffman sign indicates an upper motor neuron lesion and corticospinal pathway dysfunction likely due to cervical cord compression.
The following is a link to a video eliciting this sign:https://www.physio-pedia.com/Hoffmann%27s_SignREFERENCE:- https://www.ncbi.nlm.nih.gov/books/NBK545156/#:~:text=%5B1%5D%20The%20Hoffman%20sign%20is,to%20flex%20and%20adduct%20quickly.
Case 3
Complete details regarding the case are in the mentioned link above.ANSWERS TO CASE 31 What can be the cause of her condition ?Ans. The patient had CVT - Cortical Venous Thrombosis which occurs when a blood clot forms in the brain’s venous sinuses in smaller feeding cortical veins (cortical vein thrombosis). This prevents blood from draining out of the brain. As a result, blood cells may break and leak blood into the brain tissues, forming a hemorrhage.This patient has microcytic hypochromic anemia - Fe deficiency Anemia with her HB levels falling to even 7.7 g/dl during her hospital stay.This could possible be the primary etiology leading to her condition due to the following reasons:- Serum iron is an important regulator of thrombopoiesis. Normal iron levels are required to prevent thrombocytosis by acting as an inhibitor.
- Iron deficiency can increase the number of platelets in blood, which is linked with a Hypercoagulable state.
- Erythropoietin which stimulates megakaryocytes is also increased during the iron deficiency.
- It has been found that microcytosis decreases the cell deformability and increase the viscosity, causing abnormal flow patterns.
- Under conditions of stress or infections, the metabolic demand at the tissue level rises which can create anemic hypoxia and can predispose to venous thrombosis.
REFERENCE:
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/cerebral-venous-sinus-thrombosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3401649/#:~:text=Iron%20deficiency%20anemia%20is%20a,thrombosis%20associated%20with%20minor%20infection.
2. What are the risk factors for cortical vein thrombosis?Ans. Possible risk factors in this 17 year old could be:- Iron deficiency Anemia- Microcytic Hypochromic Anemia with HB levels falling even to 7.7 g/dl.
- Gender predisposition ( 3:1 )
- Pallor, Febrile temperature - mild infection?
- Low Random blood sugars - 75 mg/dl
- Dehydration due to vomiting episodes?
- High PT, APTT, elevated liver enzymes - defective liver function secondary to infection/disease??
Note: No other predisposing factors for CVT were present like sepsis, trauma, autoimmune diseases or prothrombotic disorders.
REFERENCE:- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6057707/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3401649/#:~:text=Iron%20deficiency%20anemia%20is%20a,thrombosis%20associated%20with%20minor%20infection.
3.There was a seizure free period in between but again sudden episode of GTCS. Why?Resolved spontaneously why?Ans. Levipil is an anti epileptic drug used to treat epilepsy seizures (fits). It works to avoid seizure as long as the patient keeps taking it.- Levipil 500 table works by reducing irregular brain activity.
- After the STAT I.V administration, there was a seizure free period due to the action of the drug and as soon as the drug action was worn out, there were episodes of GTCS.
- Then the doctor administered, Inj. Phenobarbitone which decreased the brain activity and resolved the seizure.
- Composition - Enoxaparin Sodium
- Class of Drugs - Low Molecular weight Heparin
- Type of Drug - Anticoagulant
- Mechanism Of Action - Binds to and potentiates Antithrombim (a circulating anticoagulant) to form a complex that irreversibly inactivates Clotting Factor Xa.
- Indication - Main treatment of acute venous sinus thrombosis to prevent propagation of the thrombus, pulmonary embolism, and decrease the risk of death or dependency even if there is intracerebral hemorrhage (ICH).
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6057707/
Case 4
ANSWERS TO CASE 4
1. What could have been the reason for this patient to develop ataxia in the past 1 year?
- His Chronic alcohol consumption for the past 3 years.
- Very common cause of Cerebella ataxia, affecting the gait and lower limbs more often.
- The alteration in GABAA receptor-dependent neurotransmission is a potential mechanism for ethanol-induced cerebellar dysfunction.
- Ethanol is shown to disrupt the molecular events at the mossy fiber – granule cell – Golgi cell (MGG) synaptic site and granule cell parallel fibers – PCs (GPP) synaptic site, which may be responsible for ethanol-induced cerebellar ataxia
- Molecular events at the MGG and GPP synaptic sites are mutually reinforcing and decreases excitatory output of deep cerebellar nuclei.
- His h/o multiple falls while inebriated.
- Concussion post fall and change in gait?
- His h/o unattended head injuries.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4492805/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1341444/#:~:text=The%20impaired%20platelet%20function%2C%20together,associated%20with%20excessive%20alcohol%20intake.
Case 5
ANSWERS TO CASE 5
- Early post stroke seizures, occur within 1 or 2 weeks of stroke and are thought to result from following cellular biochemical dysfunction leading to electrically irritable tissue such as:
- Acute ischemia leads to increased extracellular concentrations of glutamate, an excitatory neurotransmitter that has been associated with secondary neuronal injury.
- Recurrent epileptiform-type neuronal discharges can occur in neural networks of surviving neurons exposed to glutamate.
- The disturbance of electrolyte balance, the destruction of phospholipid membranes and the secretion of free fatty acids
- Calcium ion accumulation in hippocampal neurons has been known as a major contributor to the etiology of epilepsy.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3936028/
- https://www.ahajournals.org/doi/full/10.1161/01.str.0000130989.17100.96
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5771387/#__sec11title
- Partial seizure refers to abnormal neural activity localized to one area of the cerebral hemisphere and having a discernible focal or localized onset.
- When there is no associated impairment in consciousness, it is called simple partial seizure, and when it is associated with impairment in consciousness, it is called a complex partial seizure.
- When a partial seizure becomes generalized, it is referred to as a "partial seizure with secondary generalization."
- https://www.ncbi.nlm.nih.gov/books/NBK500005/
Case 6
ANSWERS TO CASE 6
- Meclizine, First generation antihistamine.
- Non selective H1 Antagonist with central anticholinergic effects.
- Indicated in patient's giddiness and vestibular dysfunction symptoms.
- In a double-blind crossover study, meclizine hydrochloride was shown to be significantly more effective than placebo in treating patients with positional and continuous vertigo of vestibular origin. Meclizine reduced the severity and frequency of attacks, as well as signs and symptoms associated with the vertigo. These included nausea, positional and positioning nystagmus, and postural instability.
2. Inj Zofer 4 mg IV/TID
- Ondansetron, Antiemetic, 5-HT3 Antagonist.
- Indicated for patient's nausea and vomiting.
- Nausea was significantly less in the ondansetron group within the expected duration of action of a single dose of the drug (1 hr post-anesthesia) compared to placebo.
3. Tab Ecosprin 75 mg PO/OD
- Aspirin
- Thins the blood and thereby prevents clots, is currently used to reduce the long-term risks of a second stroke in patients who've had an ischemic stroke.
- Aspirin slows the blood's clotting action by reducing the clumping of platelets. Platelets are cells that clump together and help to form blood clots. Aspirin keeps platelets from clumping together, thus helping to prevent or reduce blood clots.
- https://www.webmd.com/stroke/news/20000601/aspirin-after-stroke-helps-prevent-another
- https://www.uofmhealth.org/health-library/te7903spec
4. Tab Atorvostatin 40 mg PO/HS
- Statins lower serum cholesterol level by inhibiting hydroxymethylglutaryl-coenzymeA (HMG-CoA) reductase.
- The beneficial effect of statin therapy on the risk of recurrent stroke was due to a reduction in the risk of cerebral infarction, the mechanism of which largely has been attributed to a reduction in LDL cholesterol levels. The lower average LDL cholesterol level achieved in the atorvastatin as compared with the placebo group is consistent with this hypothesis.
- Decreased the risk of stroke, major coronary events, and revascularization procedures. These results support the initiation of atorvastatin treatment soon after a stroke or TIA.
REFERENCES:
- https://www.nejm.org/doi/10.1056/NEJMoa061894#:~:text=In%20conclusion%2C%20in%20patients%20with,after%20a%20stroke%20or%20TIA.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428028/
5. BP monitoring- 4rth hourly
6. Tab Clopidogrel 75 mg PO/OD
- Antiplatelet drug
- Clopidogrel blocks platelet aggregation through the P2Y 12 -receptor pathway, a mechanism that is synergistic with aspirin in platelet-aggregation assays.
- Combination antiplatelet therapy with clopidogrel and aspirin may reduce the rate of recurrent stroke during the first 3 months after a minor ischemic stroke or transient ischemic attack (TIA). A trial of combination antiplatelet therapy in a Chinese population has shown a reduction in the risk of recurrent stroke.
7. Inj Thiamine 1 AMP in 100 ml NSPO/BD
- Vitamin B1 supplementation.
- Necrotic cell death after cerebral ischemia triggers the activation of the immune system, followed by an inflammatory response. It is likely that fatigue related to stroke could benefit from high-dose thiamine.
8. Tab MVT PO/OD
- MethylCobalamin, Viatmin B12 supplementation.
- Mecobalamin can reduce the level of plasma homocysteine, then lead to reductions of levels of plasma inflammatory factors and volume of carotid artery plaques, resulting in more significant functional recovery.
- A high intraluminal pressure will lead to extensive alteration in endothelium and smooth muscle function in intracerebral arteries.
- The increased stress on the endothelium can increase permeability over the blood-brain barrier and cause local or multifocal brain edema.
- Endothelial damage and altered blood cell-endothelium interaction can lead to local thrombi formation and ischemic lesions.
- Fibrinoid necrosis can cause lacunar infarcts through focal stenosis and occlusions.
- Degenerative changes in smooth muscle cells and endothelium predisposes for intracerebral hemorrhages.
- Furthermore, hypertension accelerates the arteriosclerotic process, thus increasing the likelihood for cerebral lesions related to stenosis and embolism originating from large extracranial vessels, the aortic arch and from the heart.
- Adaptive structural changes in the resistance vessels, while having the positive effect of reducing the vessel wall tension, have the negative consequence of increased peripheral vascular resistance that may compromise the collateral circulation
- https://pubmed.ncbi.nlm.nih.gov/10405790/#:~:text=Hypertension%20can%20cause%20stroke%20through,local%20or%20multifocal%20brain%20oedema.
- Impaired fibrinolysis.
- Alcohol induced vasoconstriction.
- Increased platelet activation.
- Hyper homo-cysteinemia.
- Increased blood pressure and heart rate.
- Heavy consumption may acutely lead to dehydration, further increasing the transient risk of stroke.
Case 7
ANSWERS TO CASE 7
- To prevent dehydration, maintain fluid volume.
- Thiamine ( B1 ) is the primary treatment in Wernicke's encephalopathy.
- Short Acting Benzodiazepine for treating the patient's chronic alcoholism withdrawal symptoms.
- REFERENCE: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4606320/
- Anticonvulsant, anxiolytic for alcohol withdrawal symptoms
- Good efficacy, safer drug.
- REFERENCE: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5124051/
- To keep the elevated sugar levels under check, patient is a k/c/o DM type 2.
- To check for any signs of uncontrolled sugars, to avoid complications.
- To prevent complications of hepatic encephalopathy
- To combat lose of potassium and chloride ions in urine due to alcohol intake, kidney injury.
- For low levels of potassium.
- Heavy drinking makes it harder and harder to increase GABA and decrease glutamate, so more and more alcohol is required for the same outcome. Your body becomes accustomed to these changes and responds by producing more glutamate and less GABA.
- When you suddenly stop drinking, you are no longer impacting these two neurotransmitters, but your body is still over producing glutamate and underproducing GABA.
- As a result, you may become hyper excited: anxious, restless, and shaky. If you were a heavy drinker, your symptoms may be much more severe, progressing to tremors, seizures, and serious high blood pressure.
- As thiamine blood levels fall, thiamine-dependent enzyme systems involved in prevention of cellular damage become impaired and metabolic demands increase, which can result in selective brain lesions correlated with Wernicke’s encephalopathy.
- Consequently, thiamine deficiency and development of WKS is particularly prevalent in malnourished patients oftentimes due to the shift in diet away from vitamin-rich foods and, as in the case of chronic alcoholism, a shift towards the carbohydrate-heavy consumption of alcohol.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5354137/#:~:text=Wernicke's%20encephalopathy%20is%20an%20acute,nystagmus%20and%20ophthalmoplegia%20(1).
- Ethanol itself markedly induces the expression of the microsomal ethanol oxidation system (CYP2E1), producing reactive oxygen species as a byproduct.
- Increased gastrointestinal permeability and endotoxin load may lead to alcoholic steatohepatitis resulting in excessive immunoglobulin A (IgA) load (due to increased intestinal production and decreased hepatic IgA clearance).
- IgA deposits may accumulate in the kidney, leading to glomerulopathy. Renal microcirculatory alterations in advanced liver cirrhosis leads to hepatorenal syndrome.
- Alcohol-induced skeletal muscle damage leads to excessive amounts of circulating myoglobin, causing renal tubular injury as a result of increased oxidative stress. Due to the development of alcoholic cardiomyopathy, chronic renal hypoxia develops, activating the renin–angiotensin–aldosterone system (RAAS), which in turn leads to further free radical production and to the propagation of fibrotic pathways.
- Increase in pro-inflammatory cytokines and iron dysregulation - Alcohol, Diabetes, Smoking, poor nutrition, malabsorption.
- Inappropriate erythropoietin (EPO) levels or less response to erythropoietin - Alcohol effects on Bone marrow, kidney dysfunction.
- Decreased RBC survival and Bone Marrow Infiltration - Bone marrow toxicity due to alcohol dependence and smoking.
- Poor blood flow in the extremities.
- Peripheral Arterial disease, Peripheral Neuropathy
- Decreased tissue perfusion and oxygenation due to toxic by products such as carbon monoxide, hydrogen cyanide, etc.
- Nicotine - Affects osteoblasts and delays bone healing, decreased tissue perfusion.
- Poor nutrition impairs wound healing.
- Ethanol exposure can lead to impaired wound healing by impairing the early inflammatory response, inhibiting wound closure, angiogenesis, and collagen production, and altering the protease balance at the wound site.
- https://www.researchgate.net/publication/301827503_A_study_on_the_impact_of_smoking_and_alcoholism_as_determinant_factors_in_the_prognosis_and_outcome_of_diabetic_foot_ulcer_disease
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2903966/#:~:text=In%20summary%2C%20acute%20ethanol%20exposure,balance%20at%20the%20wound%20site.
Case 8
ANSWERS TO CASE 8
- Diuretic Therapy
- Female gender
- Alcohol Intake
- Inadequate intake - anorexia, malnutrition, starvation
- Diarrhea, Excess vomiting
- Hypertension
- Heart failure
- Alkalosis, Mi, Head injury
- Cushing's Syndrome
- Respiratory Alkalosis
- Cystic fibrosis
- Excessive sweating
- Severe Burns
- Transcellular shifts - Diabetic Ketoacidosis
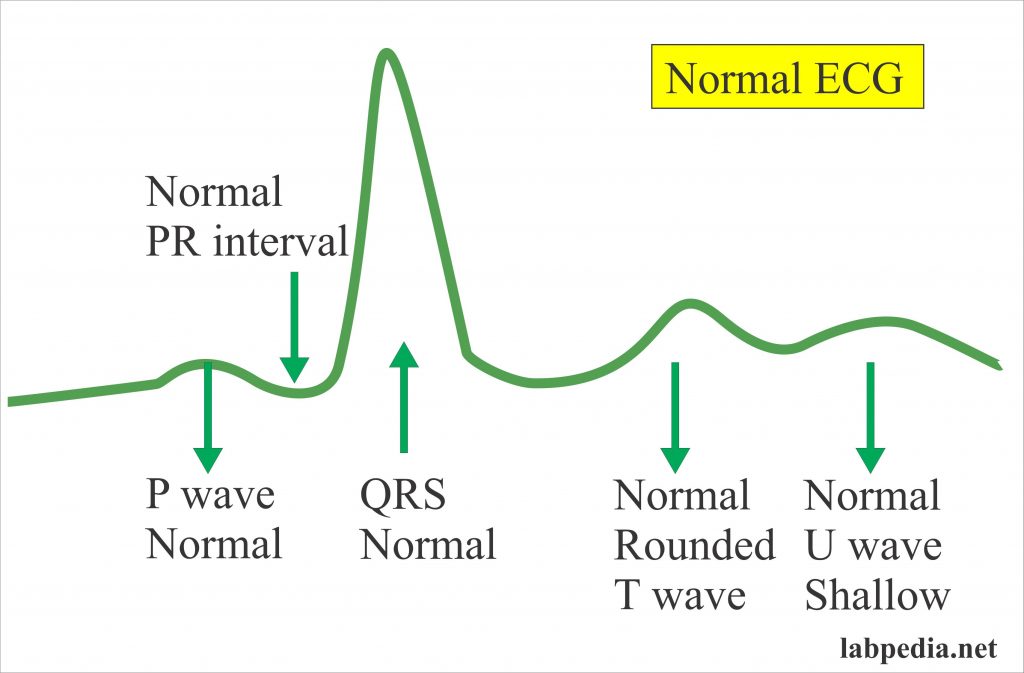
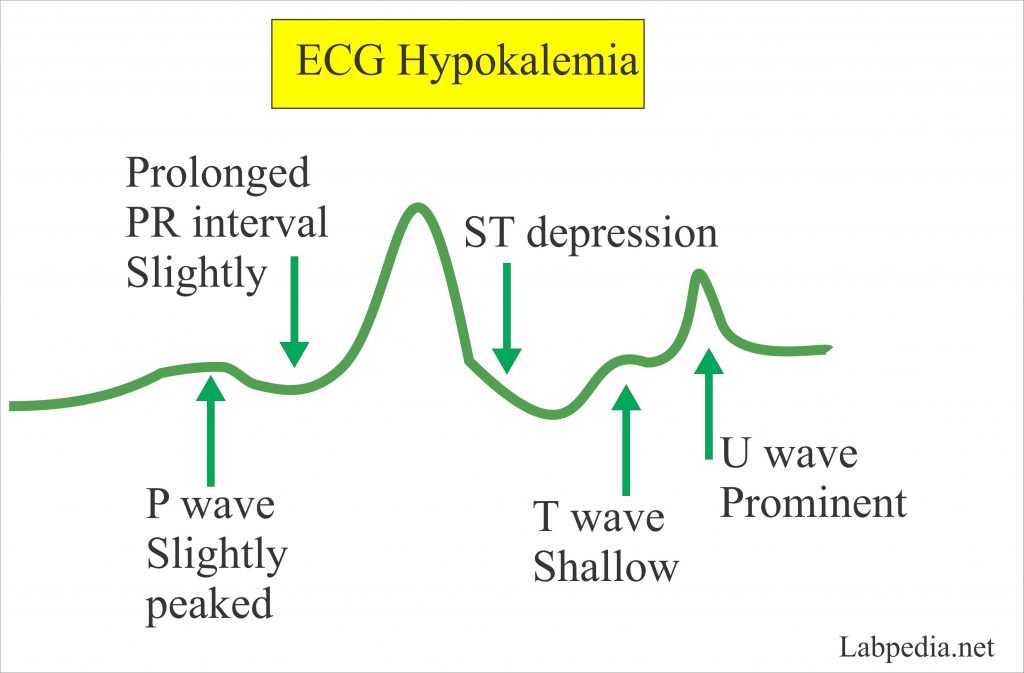
- Changes in ECG in Hypokalemia:
- T – waves are depressed.
- P – wave has peaked.
- ST – depression.
- U- wave is prominent.
- Changes in ECG in Hypokalemia:
- Potassium level < 2.5 meq/L
- There will be tachycardia.
- There is increased muscular irritability.
- There are specific cardiac conduction defects.
- There is stoppage of the heart in the systole.
- There is a flattened T – wave.
- The end result will be cardiac arrest.
- Potassium level <3.0 meq/L - There are marked neuromuscular symptoms.
INFECTIOUS DISEASES
Case 1
ANSWERS TO CASE 1
- Medial canthus, eyelids, periorbital area
- Hard palate
- Sinuses, Left nasal cavity
- Lipid formulations of amphotericin B (LFAB) have evolved as the cornerstone of primary therapy for Mucormycosis.
- LFABs appear to be less nephrotoxic, safer, efficacious alternatives to AmB for the treatment of Mucormycosis.
- Better CNS penetration than AmB and improved outcomes vs. AmB in murine models and a retrospective clinical review.
3. Deoxycholate amphotericin B (AmB)
- >5 Decades clinical experience.
- Inexpensive.
- Only licensed agent by US Food and Drug Administration for the treatment of Mucormycosis.
- Improper use of steroids - too early, excess dose, prolonged period.
- Poor Management of Diabetes.
- Late diagnosis of Diabetes.
- Over diagnosis and over treatment.
- Lack of a strict prescription check.
- Improper use of oxygen cylinders - outdated tanks, unclean masks and unpurified water in the apparatus.
- https://qz.com/india/2012257/why-india-has-so-many-cases-of-mucormycosis-or-black-fungus/









Comments
Post a Comment