32Y Male with FEVER and DYSPHAGIA since 1 WEEK
Introduction: This is an online E-log Entry Blog to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs.
CHIEF COMPLAINTS:
1. Fever since 1 week.
2. Difficulty in swallowing since 1 week.
HISTORY OF PRESENTING ILLNESS:
- Patient was apparently asymptomatic 6 years back when he met with an accident (RTA - bike vs lorry) and sustained following injuries:
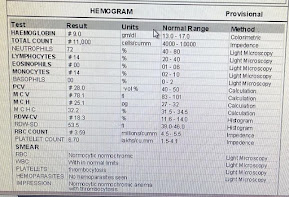
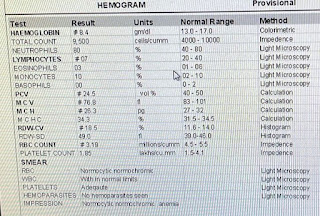
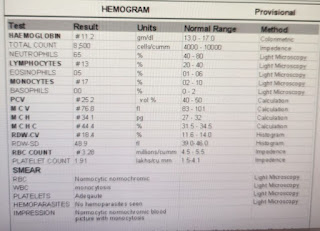
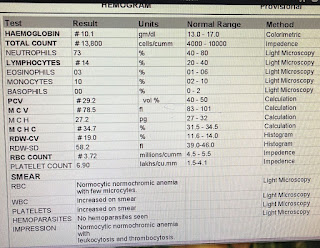
- Hemoglobin: 10.6 g/dl (Normal 13-16gms)
- Total RBC Count: 4.60 million/cumm (Normal 4.5-6.5 mill)
- Platelet Count: 5.98 Lakhs/cumm (Normal 1.5-4lakhs)
- Total WBC Count: 22,500/cumm (Normal 4,000-11,000/cumm)
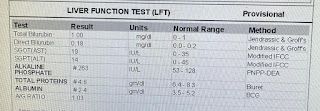
- Total Bilirubin: 0.7mg/dl (TB Normal 0.1-2mg)
- Malaria Test: Negative
- Widal Test: S Typhi "O" Positive (1:160) , S Typhi "H" Positive (1:80)
- Hemoglobin: 8.1 g/dl (Normal 13-16gms)
- Total RBC Count: 2.7 million/cumm (Normal 4.5-6.5 mill)
- Platelet Count: 2.4 Lakhs/cumm (Normal 1.5-4lakhs)
- Total WBC Count: 13,300/cumm (Normal 4,000-11,000/cumm)
- RBS: 158mg/dl (Normal 80-170)
- Blood Urea: 55mg/dl (Normal 14-45)
- Serum Creatinine: 2.89mg/dl (Normal 0.6-1.2)
- Patient is a known case of Diabetes Mellitus type 2, since 6 months, on T Glimiperide 1mg + T Metformin 500mg.
- Patient is not a known case of Hypertension, Thyroid disorders, Seizures, Tuberculosis, Asthma, stroke or any cardiac disorder.
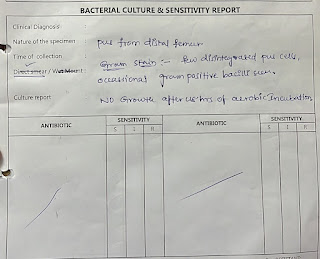
- History of previous surgery - Nailing for Femur fracture and Plating for Tibia fracture, 6 years ago.
- His appetite has decreased since past 1 week, he consumes a mixed diet, sleep is disturbed
- Bowel movements are normal but Decreased urine output since the last couple of days whenever fever spiked.
- No history of smoking or alcohol.
- No known food or drug allergies.
- No similar complaints in the family members.
GENERAL PHYSICAL EXAMINATION:
Examination has been done in a well-lit room in supine and sitting posture after taking informed consent and after reassuring the patient.
- Patient was conscious, coherent, co-operative and well oriented to time, place and person.
- Moderately built and nourished.
- Pallor present.
- No signs of Icterus, Cyanosis, Clubbing, Pedal edema, Generalized Lymphadenopathy.
- JVP normal.
Central Nervous System: No abnormality detected.
Per Abdomen: Soft and nontender, no organomegaly.
Cardiovascular System: S1, S2 heard, no murmurs
Respiratory System: BAE+, NVBS +
22/06/2023
Temperature - 99.6F (two fever spikes in the night)
Respiratory Rate - 23 cpm
Pulse Rate - 110 bpm
Blood Pressure - 100/70 mm Hg
SpO2 - 99 at room air
23/06/2023
Temperature - 99.4F
Respiratory Rate - 22 cpm
Pulse Rate - 115 bpm
Blood Pressure - 110/70 mm Hg
24/06/2023
Temperature - 100.4F
Respiratory Rate - 24 cpm
Pulse Rate - 108 bpm
Blood Pressure - 100/60 mm Hg
Input/Output - 2400/900ml
25/06/2023
Temperature - 100.2F
Respiratory Rate - 22 cpm
Pulse Rate - 120 bpm
Blood Pressure - 100/60 mm Hg
GRBS @ 8Am - 300mg/dl 10 units HAI and 6NPH given
Input/Output - 3700/1200ml
- BLOOD UREA: 55MG/DL (Normal 12-42)
- SERUM CREATININE: 1.2MG/DL (Normal 0.9-1.3)
- C REACTIVE PROTEIN: POSITIVE 1.2MG/DL (Normal 0.3-1)
- Serology Rapid HBsAg/HIV1/2/Anti HCV - Negative
- RBS: 115mg/dl (Normal 80-170)
- BGT: O Positive
- LFT's:
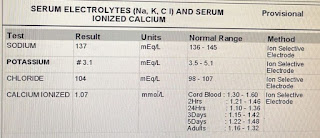
1. Spot Urine Sodium: 123mmol/L
2. Spot Urine Potassium: 6.6
3. Urinary Chloride: 154mmol/L
4. HBa1C: 6.7%
5. FBS: 227mg/dl
6. Blood Lactate: 6.9mg/dl
7. LDH: 190 IU/L
8. PT/INR: 18sec/1.30
9. APTT: 35 sec
- Blood Urea: 14mg/dl (Normal 12-42)
- Serum Creatinine: 0.9 mg/dl(Normal 0.6-1.2)
- PLBS: 196mg/dl
PROVISIONAL DIAGNOSIS:




















































































Comments
Post a Comment